Cancer Prehabilitation Service - Nottingham University Hospitals NHS Trust
Winner – Partnership Working to Improve the Experience and Personalisation of Care

Contact: Abi Burrows - abi.burrows@nuh.nhs.uk
Organisation
With more than 18,000 colleagues, Nottingham University Hospitals NHS Trust (NUH) is the largest employer in Nottinghamshire and one of the biggest and busiest acute NHS Trusts in the country, serving more than 2.5 million residents of Nottingham and Nottinghamshire and a further four million people across the East Midlands and beyond.
NUH is a key member of the Nottinghamshire Integrated Care Board (ICB) and has built strong relationships across organisations and boundaries. We are proud of our collaborative culture and recognise the key role these collaborations play in helping to improve the health and wellbeing of citizens that live and work in the area.
General Summary

NUH launched a new cancer Prehabilitation Service in April 2022. Co-designed with patients from the outset, the purpose of the service was to prepare patients ahead of their cancer surgery through improvements in physical fitness, psychological wellbeing and healthy eating. Research has demonstrated this approach can reduce length of stay, limit post-operative complications and support enhanced recovery.
The value of this service is system wide, achieved through a unique collaboration of health, social care, and independent and third sector partners to deliver a personalised care approach. We worked with our patient and community partners to empower patients to make key behaviour changes and maintain positive outcomes beyond their acute treatment. The creation of strong community networks has helped to improve the long-term health and wellbeing of our local communities.
We are proud of the strong relationships and sense of team developed through the creation of this integrated pathway. Evidenced by the improved patient outcomes, delivery of efficiency savings and positive feedback we receive from patients and their families at every step of the pathway. We are seeking to share these achievements and learning to inspire others and enthuse our own team to future improvements.
Rationale
Significant postoperative complications currently occur in up to 75% of patients undergoing major cancer surgery. This is increasing due to the trend in acknowledged risk factors, which include an aging population, frailty, obesity and presence of multiple existing comorbidities. These serve to delay recovery and place a significant psychological burden on the individual while simultaneously placing additional strain on healthcare resources.
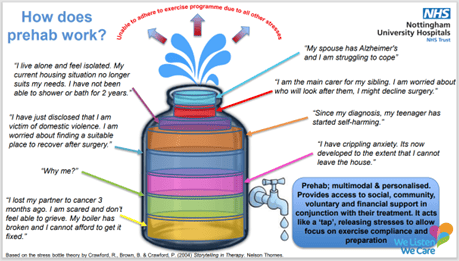
Prehabilitation (prehab) provides support to patients to maintain their physical and psychological wellbeing to cope with cancer treatment. This is achieved through promoting healthy behaviours and improving cardiovascular fitness, nutrition and psychological interventions, maximising any available time before surgery. This early intervention provides an opportunity to optimise patients through both medical interventions and to address patient’s individual needs, such a financial, housing and social support.
The evidence base behind prehabilitation is evolving rapidly and has already shown reduction in mortality, complications and length of stay as well as providing an opportunity to improve long-term health. A randomised controlled trial from Barcelona that showed prehab in high-risk surgical patients reduced major complications by 50% and a 2022 independent report into Manchester’s Prehabilitation program (Prehab4Cancer) found a 1.5-day reduction in hospital length of stay (LoS) and a 0.4-day reduction in critical care length of stay per prehab patient. It can help to tackle health inequalities and is aligned with personalised care agenda in the NHS Long Term Plan and NICE guidance. Consequently, prehabilitation is now a key GIRFT (Getting It Right First Time) recommendation to improve a patient safety during and after surgery and reduce post op complications and readmissions and is viewed nationally as a quality standard for cancer care.
As well as delivering these immediate benefits for patients, the team’s longer-term aspiration of the service was to contribute to an overall improvement in long-term health and wellbeing of our local population by empowering patients to maintain positive lifestyle changes. This involved working with community partners to embed participation in exercise beyond that of prehab and encourage peer support networks.
Planning
From the outset the team recognised the value of including patient representatives in the design process, formally inviting two patients’ partners to join the co-design team. Lizzie and Robin, both cancer survivors provide lived experience of cancer and some of the treatments involved.
Partnering with ‘A Better Life’ (ABL) has enabled us to be able to offer community based group sessions. ABL is a provider of health and well-being services, using a community-centric delivery model. This partnership has meant patients can attend clinics in their community, reducing travel time and associated expense. Furthermore it can reduce the stress and anxiety patients can experience when contemplating travelling an extenxed distance or multiple public transport routes.
Working in collaboration with the Clinical Psychology Cancer Service based at a neighbouring Trust, the team have been able to develop a dedicated direct referral pathway that ensures patients requiring a higher level of psychological support are seen with 2 weeks of referral, providing access to a video psychotherapy service.
We also partner with Self Help UK who provide Social Prescriber Link workers to support with the management of our patients social and psychological needs. Without this, some of our patients would not have been able to participate in prehab and ultimately go on to receive their surgery. For example, an agoraphobic patient, unable to leave the house following the death of her partner, received emotional support from volunteers to help manage her anxiety and attend appointments.
Our patient partners highlighted the frustrations they had experienced in having to repeat their story to different health care professionals. We worked with digital colleagues to set up a bespoke electronic information sharing process, which minimises the risk of patient information being lost and patients having to repeat their information to multiple providers, creating an integrated patient record. This automatically shares information between partners and uploads partner information into the hospital record providing two-way communication
A repeated theme of feedback was our patient’s desire to continue with exercise sessions after their surgery (rehabilitation). The team approached the Cancer and Rehabilitation Exercise (CARE) team, an established Cancer rehabilitation programme provided by Nottinghamshire County FC, Notts County Foundation. NUH and CARE have now developed an integrated pathway, which offers transitional rehabilitation sessions to ensure a seamless transition from ‘Prehab to Rehab’, with familiar faces, in a familiar environment, breaking down potential barriers to accessing rehabilitation.
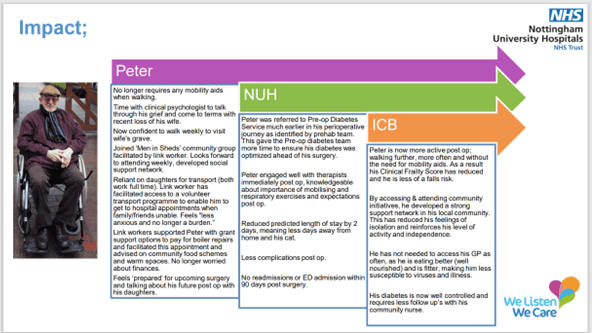
Impact
In the 15 months since the service launched, we have seen significant improvements against all the outcomes measures, both physical and psychological. On average;
- Grip Strength (Left)- increased by 1.5kg
- Grip Strength (Right)- increased by 1.9kg
- of sit to stands in 60 secs increased by 6.2
- Incremental Shuttle Walk test (change in m walked) increased by 49.5metres
- of minutes mod/strenuous physical activity per week increased by 144 minutes
- of Strength Sessions per week increased by 2.3
- EQ-5D-5L health score (change in wellbeing) improved by 2.4
- Depression score(PHQ-9) decreased by 2.4
- Anxiety score (GAD-7) decreased by 2.1
- Alcohol Intake (units) decreased by 2.2 units.
Patient and Staff Feedback
In addition to quantitative measures, we collected patient and staff feedback throughout. Unanimously our patients describe feeling more physically and mentally prepared and regaining a sense of control.
Long Term Health/System Benefits
Early indications from 3-month follow up data show that improvements in activity levels are sustained into the post-op period. 27% of patients report being more active within three months post-surgery than before entering the service.
Financial Efficiency
From a hospital perspective, we measure the total length of stay (LoS) and time in a HDU level 2 beds post operatively, compared to the same Health Resource Groups (HRG) historically. This has demonstrated a mean per patient reduction of 1.2 days and 0.5 days respectively, releasing bed capacity to improve flow and support elective recovery. We have also seen a reduction in readmissions and emergency admissions (ED) within 90 days post-surgery of Prehab patients compared to the same HRGs historically.
The Future
Following the successful launch of the service there have been multiple requests from surgeons and anaesthetic colleagues from specialities across the Trust to expand our service to include benign (non-cancer) surgical patients, which has led to the creation of a business case currently going through internal Trust governance processes. We intend to identify and positively discriminate towards those in social deprived areas using the indices of social deprivation (ISD).
A member of the prehab team sits on the Nottinghamshire ICB for Personalised Care group to share insight and learning and the service has recently been asked to support in the creation of Prehabilitation guidelines for the British Gynaecological Cancer Society.
A further piece of work currently being progressed is the development of early screening and health optimisation for all inpatient pathways by April 2024 as part of a new NHSE mandate and is heavily influenced by prehabilitation principles and learning.
The addition of the Exercise Physiologists to the Trust has allowed the service to offer the first placements for Sports Rehabilitation students. This supports role development and succession planning.
Standing Out
Delivery of this cost effective, holistic offer has been achieved by integrating with our community partners’ established infrastructure, minimising costs and providing access to a range of physical, psychological health and care services. Working with Local Authority partners has achieved an ICS cost saving of £60k by using existing underutilised commissioned capacity. This allows us to offer support to a larger cohort of patients within limited resources.
Our partnerships have improved accessibility for patients by offering community based choice and care closer to home. 45% of participants completed structured exercise programmes in six local leisure centres as an alternative to hospital. Our partnership with ABL allowed us to achieve a waiting time standard of three days by increasing capacity that would not be possible within the hospital resources. This allows the hospital team to focus on those with the most acute needs.
One of the unique characteristics of our service is the inclusion of dedicated social prescriber link workers, with 30% of patients accessing their support in the first 12 months. A repeated theme we hear from patients is that they feel able to discuss concerns with Social Prescribers, which they would not have raised with their clinical team, not perceiving them as medically relevant. This ability to ‘off load’ worries and share concerns helps to improve confidence and ability to participate in the wider prehab offer and is intrinsic to the service achieving the positive improvements.
Key Learning Points
- Patient Partners provide valuable insight and knowledge; they are worth their weight in gold!
- Do not underestimate the volume of communication required when launching a service and allow time for a service to become embedded.
- Development of new roles, recruitment and governance all takes time but are the key foundations to a successful service.
- Networking, linking in with the colleagues across the systems and sharing practice are an essential part of collaboration and partnership working
- Whilst data and financial impact remain essential, patient stories are extremely powerful and the patient voice must play an equal part in demonstrating impact.
