Modernising Medication Management in a Prison Setting
Serco Justice & Immigration

Contact: Hayley Peek - Hayley.Peek@serco.com
Organisation
Serco manages custodial services across the justice system on behalf of the Ministry of Justice (MoJ) and Scottish Prison Service (SPS). We operate six adult prisons in the UK and constantly and systematically look to make change for the better, putting the needs of prisoners, colleagues and communities at the heart of service design, while working within established policy frameworks and observing complex regulatory, security and governance requirements.
HMP Dovegate is one of the prisons we manage. It’s a Category B adult male facility with up to 1,060 male adult prisoners serving a range of sentences including trial, remand, those awaiting sentence and convicted men serving long and short-term sentences. HMP Dovegate has the UK’s only privately run purpose-built therapeutic facility. The therapy that’s offered helps offenders stop their pattern of offending.
Practice Plus Group (formerly Care UK) is a leading provider of independent healthcare; providing predominantly NHS Services. As a large organisation with a national footprint, we employ in excess of 6000 staff to deliver safe and high-quality healthcare services in line with our ethos of ‘Access to Excellence’.
Healthcare services in prisons are commissioned directly by NHS England and we currently operational in 47 prisons of all categories nationally; delivering healthcare to over 40,000 patients, all with very unique, and often highly complex healthcare needs, including HMP Dovegate. In partnership we strive to ensure that Prisoners receive equivalent healthcare services within HMP Dovegate and have worked collaboratively on this initiative purely for the benefit of prisoners.
General Summary
Overall Insight Category Winner
Winner – Partnership Working to Improve the Experience
Runner Up – Innovative Use of Technology, Social, Digital Media
Managing prisoners’ medications is challenging due to greater degrees of health needs when compared to the general population. To improve prisoners care and meet the needs of our population, we needed a better understanding of medication management challenges and to consider how to resolve them, whilst retaining a high level of care equivalent to a community setting and ensuring staff safety.
Following detailed research and design thinking, an innovative pilot project was undertaken to enable independent collection of in possession (IP) medication. A locker system was designed and tested within the TC* facility at HMP Dovegate. Results have been extremely positive and related to improved patient safety and effective governance, this includes a 16% rise in the number of prisoners who can now have their medication in-possession. All stakeholders reported improvements against proposed project benefits, with themes emerging around:
- Better access to medications,
- Improved patient management/ control,
- Reduced delays (staff/ patients)
- Improved accuracy, time management, partnership working and governance.
This project was highly ambitious, considering the security requirements of prisons, which are challenging places to implement technological innovations. Not only has this partnership achieved this, but also has set the blueprint for further roll-out nationally.
Rationale
Medication plays an essential part in prison healthcare and demand has soared in recent years. Reasons for the increase include:
Increasing prisoner numbers
- The aging prisoner population. Prisoners over the age of 50 increased from 4,800 in 2002 to nearly 12,600 in 2016)
- Increases in poor health and long-term conditions requiring prescription medicines
- National increases in medication usage
- Increases in the number of medicines classified as Scheduled Controlled Drugs requiring supervised administration.
- Trading/ diversion of medications whereby prisoners may sell/divert high risk medication, such as Tramadol & Pregabalin, into the illicit prison economy presenting a significant risk of harm to both our staff and prisoners who have to respond to the side effects, bullying and/or in some cases, overdose scenarios.
Consequently, large volumes of medications are routinely prescribed and dispensed. They are taking longer to deliver, resulting in a negative experience for prisoners (The Kings Fund, 2020). Medications management has also consistently been the area of most complaints for healthcare providers in prisons.
Following a suitable risk assessment, prisoners can manage a range of medications in-possession (IP) and store them independently (in line with how we would normally manage medication in the community). However, some medications, such as controlled drugs, must be supervised by healthcare professionals because evidence and experience points to specific risks, such as misuse, polydrug use, trading of prescribed medications, bullying, and not complying with medication regimes. These are not in-possession (NIP) drugs and were the focus of this innovative project.
Supervising medication dispensing by both custodial and healthcare staff has created an increased demand on services within the prison leading to:
- Increased time waiting for medication
- Missing medication doses, impacting clinical management and safety
- Violence flashpoints
- Diversion or bullying
- Often medication takes a long time to administer so prisoners are left missing out on other areas within their day, such as work, education, gym, faith, healthcare appointments and access to wellbeing activities (such as fresh air and socialising opportunities)
- Regime delays for others if medications overrun
- Complaints
- Insufficient resources or strain on existing clinical and custodial resources
- Poor prisoner and staff experience
The scale of the challenges are such that previous changes to the service delivery model have been unsuccessful in achieving sustainable improvements to this vital area of care. Consequently, we looked to technology to help solve what is a growing problem with the aim of improving service delivery for prisoners and all staff.

Planning
Due to the nature and complexity of this project there were several phases, comprising of problem definition, baseline assessments and planning, followed by design and implementation.
- Site selection – The TC* in Dovegate prison was selected as it was representative of a Category B prisoner population, the population was stable and the infrastructure was appropriate i.e. IT connection, accessibility, space and security infrastructure.
- Pre- implementation questionnaire and focus groups among prisoners and staff – demonstrated that the overall experience of queueing, receiving and dispensing medication in prison was not satisfactory:
- A significant proportion (65%) felt current processes prevented them from choosing their daily activities such as exercise, eating, work and exercising.
- 61% of respondents were unlocked to collect medication in under 20 minutes, 25% waited from 20-40 minutes and 14% waited in excess of 40 minutes
- 68% reported waiting in the medication queue between 0-20 minutes, 25% waited between 20-40 minutes and the remaining 7% waited in excess of 40 minutes.
- Medications were also considered one of the most difficult and stressful services to deliver in the prison by custodial and healthcare staff prison setting
- Design and install a cutting-edge locker design with biometric fingerprint access linked to the prison scheduling system to enable the remote collection of In-Possession medication. The solution allows prisoners autonomy in collecting their medication and therefore more independence and self-care. They are informed of when they are able to collect their medication, as they would in the community, giving them choice in how they structure their day.
The solution was developed and piloted in consultation with a wide-ranging multidisciplinary project group (custodial, nursing, pharmacy, IT, engineering, Facilities Management and prisoners). Based on the feedback received the solution was continually adapted and refined to deliver the best experience for service users and staff.
Impact
The design, build and installation of the Medication Dispensing Lockers* (MDL) solution was evaluated both qualitatively and quantitatively.
- Post- implementation focus groups (prisoners and staff).
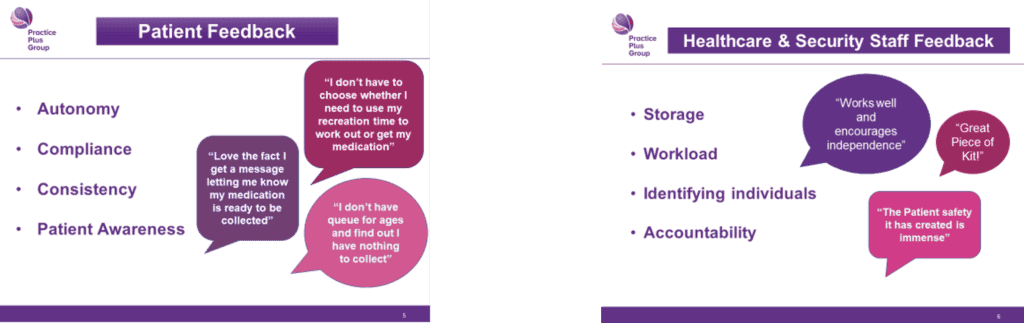
Prisoners – were extremely positive and felt the experience of collecting medications was greatly improved. Key themes were that the MDL*:
- Freed up time for custodial staff, improving overall access to available services.
- Is less disruptive
- Faster
- Allows flexibility, enabling prisoners to collect their medication at convenient times
- Reduced disruption to other essential prisoner activities, as the need to queue is greatly reduced
- Is more reliable
- Provides clarity around when medication is ready as prisoners are notified via the prison messaging system that medications have been loaded. Previously there was no mechanism to inform prisoners that their medication was ready.
- Reduces stress and time burden for the prisoners compared to the previous processes
- Reduces anxiety and concerns in relation to medications collection
- Increases prisoner’s independence and control of medications
- Improves privacy and decency
- Increases uptake and collection of medication.
- The locker medication cleardown process results in uncollected medications being easily identified and followed up as appropriate. Previously this was manual process dependant on staff consistency, which could be difficult to maintain.
Custodial staff – felt that the system was a positive development in the management of medications. Key points were:
- Flexibility that the MDL* offered around activity management
- Reduced queries on when medications were available as notifications were available via the prison messaging system
- Reduced missed medications
- Saved staff and prisoner time, allowing custodial staff time to complete other tasks
- Improved safety by reducing prisoner frustrations relating to medications management
- Reduced staff stress
Quotes from the staff group included “it saved 45 minutes”, “changed ops delivery of meds”, “I am able to fulfil my role requirements” and “much better for residents”.
Healthcare staff
A cross selection of multidisciplinary staff (pharmacy and nursing) participated in focus groups. Under the previous system there hadn’t been the ability to notify prisoners that medications had arrived, and the infrastructure was limited in storage options. In their view the MDL* solution improved the whole medications administration process, allowing more effective interactions with residents, reducing abuse.
Key themes were:
- Accurate
- Quicker for nursing, less stressful and easier to locate non-IP medication
- Improved space and storage
- Improved/ more compliance in prisoners collecting medication
- Reminder on CMS (improves communication and reduces frustration)
- Reduced wait times for prisoners
- Improved privacy
- Decreased drug errors as biometrics improves patient identification process, for example for patients with same names
- Improved responses to enquires – queries can be sent directly to pharmacy rather than relying on nurses to relay them to pharmacy
- Less opportunities for prisoners to divert supervised medications at the hatch due to reduced activity.
- Increases prisoners’ self-management of medications
- Audit process improved
Post- implementation survey of users
– 80% of those who answered the survey thought the MDL* was easy to use
– 92% were positive about the experience of using the MDL*
– Only 14% would like to see improvements. Many of the suggested improvements were outside the project scope and related to the wider medication pathway i.e. automated reordering, repeat prescriptions, wider rollout in the prison.
Standing Out
What started as an operational challenge, quickly developed into improving the experience of medication management for prisoners and staff, with numerous partner agencies fully committed to supporting a necessary but significant change. This is particularly important as health needs amongst people in prison, tend to have a greater need for healthcare and the MDL increases the opportunity for prisoners to take control of their medication and also supports clinical staff to delivery all aspects of care delivery rather than just focusing on medications administration.
This concept is highly innovative, has not been utilised elsewhere and embracing technology to increase the efficiency of a process has benefitted all stakeholder groups, whilst also returning an important part of quality delivery – time and choice. Both of which can be better spent accessing services such as Education, Sport, Faith etc.
Key Learning Points
Incorporating service users and key stakeholders feedback across all stages has been crucial, with feedback resulting in design and functionality modifications.
Early engagement with service users, has also been invaluable ensuring the best design and also ongoing engagement with the change. Service user representatives are now being trained to support wider rollouts.
