Bereavement Support Service
Calderdale and Huddersfield NHS Foundation Trust
Contact: Gillian Sykes - gc.sykes@hotmail.co.uk
Organisation
Calderdale and Huddersfield NHS Foundation Trust employ more than 6,000 staff who deliver compassionate care from our two main hospitals, Calderdale Royal Hospital and Huddersfield Royal Infirmary, as well as in community sites, health centres and in patients’ homes. We provide a range of services including urgent and emergency care; medical; surgical; maternity; gynaecology; critical care; children’s and young people’s services; end of life care and outpatient and diagnostic imaging services. We provide community health services, including sexual health services in Calderdale from Calderdale Royal and local health centres. In 2019/20 we cared for more than 119,000 men, women and children as inpatients (stayed at least one night) or day cases. There were also more than 445,000 outpatient attendances; 154,000 accident and emergency attendances and 5000 babies delivered. There were some 261,000 adult services contacts by our community teams as well as 217,000 contacts with our therapy services.
General Summary
The Bereavement Support Service is a unique collaborative initiative with bereaved relatives at its heart. The service has 2 elements:
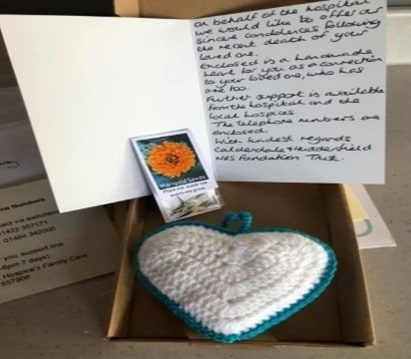
- A bereavement box is sent to families of deceased patients – it contains marigold seeds, a handwritten card, bereavement support numbers and a knitted heart. Relatives are made aware that a knitted heart is placed with the deceased patient.
- Calls to relatives – take place 5-10 days after the death.
The service was developed in response to the passion of Trust staff and feedback from our local community. The service is innovative and epitomises the Trust’s vision ‘Together we will deliver outstanding compassionate care to the communities we serve’. It was set up to support bereaved relatives at unprecedented times and the fantastic feedback received both from staff providing the services and relatives has made it clear that this service is hugely appreciated and one that we intend to continue.
The service has clear operational goals, is delivered through a committed workforce and the Trust is fully supportive. The initial aim of the service was to provide support for bereaved relatives. It has also enabled the Trust to respond quickly to feedback provided, sharing positive messages, and addressing learning opportunities.
Rationale
The country went into lockdown in March 2020 due to Covid and following government guidelines Trusts were advised to cease patient visiting immediately. Staff expressed concern that patients were dying alone which may cause relatives to have lasting distress and unresolved grief. We also had feedback and concerns highlighted through the Patient Advice and Complaints department about end of life care.
The Trust agreed to look at what extra bereavement support could be introduced to provide a workable, equitable, organised support system for all bereaved families. The new Bereavement Support Service was for relatives of all adults (over 18) that die in the Trust – exceptions were ICU patients, where support was already in place.
The Trust has 4 recognised behaviours, known as our ‘four pillars’. The way this project was co-ordinated clearly demonstrated these:
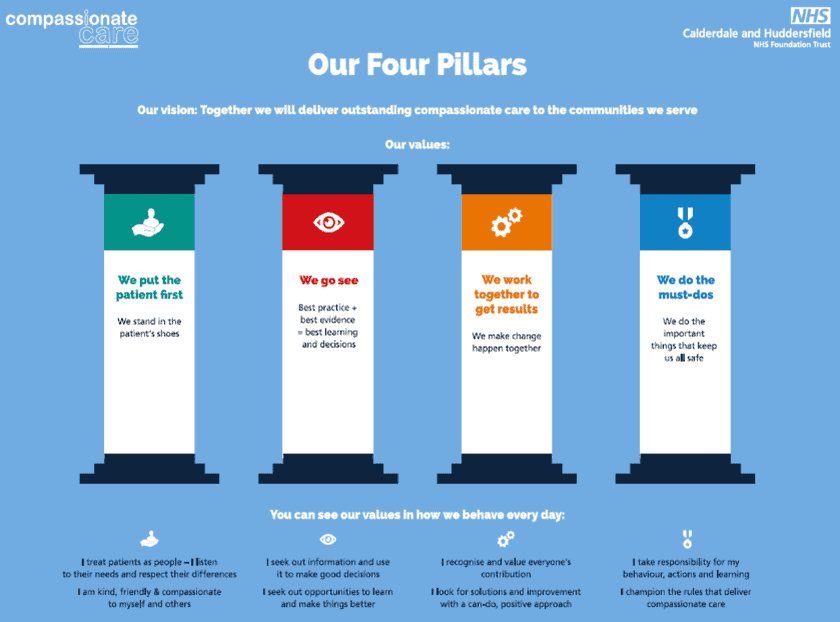
- We put the patient first – in this case the bereaved relatives
- We go see – identifying evidence of what comforts and supports relatives to manage their grief
- We work together to get results – a team to agree the scope and a team to deliver the initiative came together
- We do the must-dos – a support separate from the ward staff enabled the front-line teams to focus on direct patient care; ensured the system introduced was compliant with GDPR – advised by Information Governance team.
Planning
The project lead brought together a working group to review ideas gathered from colleagues to devise a plan for what the additional support for bereaved relatives would be and the resources required.
It was agreed the End of Life Care team (EOLCT) were best placed to co-ordinate and manage this new support rather than at ward level. The team benefited from the use of redeployed staff to enhance the service, enabling staff who were unable to contribute to direct patient care to continue to use their skills.
To support staff joining the team and provide assurance that those making the calls were following the required process a Standard Operating Procedure was developed. New staff shadowed experienced colleagues and where staff found calls challenging the EOLCT followed up.
The potential emotional impact on these staff was acknowledged, including by the Trust’s Patient Experience and Caring Group which formally recognised the ‘fantastic job’ and enquired if there was support required from the organisation. This was co-ordinated via the Trust’s Health and Wellbeing offer and the Trust Psychologist.
From previous experiences the EOLCT knew offering relatives a number to call for support was unlikely to achieve many calls therefore the team were keen to make proactive phone calls. Through experiences of running an Experience Based Co-design (EBCD) bereavement workshop the team knew a personal handwritten card rather than a printed one was preferred.
Key components of the service were specified and an assessment of who was placed to deliver these. The following are now an integrated part of the project delivery team:
- Clinical Governance Team: daily administration support
- General Office: provision of relatives’ details
- Mortuary: placing hearts with deceased patients
The content of the box was agreed as – handwritten card, marigold seeds, bereavement support telephone numbers, a handmade heart and information that a heart was also placed with the deceased patient. Telephone calls were made to the Next of Kin (NOK) 5-10 days after the death. Any feedback for the ward is timely, with an agreement to ring the relatives and address issues immediately rather than letting problems potentially worsen, with a follow up call from the Bereavement team to ensure issues had been dealt with. The team supports staff who have struggled with deaths on the wards by providing 1-1 meetings and signposting to the Trusts health and wellbeing initiatives.
Impact
Since March 2020 the Trust has had 1949 deaths and 1710 (88%) boxes have been distributed and 1239 (64%) phone calls made to bereaved relatives with follow ups and referrals onto different professionals too. As this was a service set up in response to the Covid pandemic it hasn’t been possible to provide quantitative benchmarked measures. Outcomes to date have been measured through qualitative feedback which has described the impact for relatives and staff involved in the process:
Examples of relatives’ feedback:
- “Heartfelt thanks for the card and heart, I loved that the card was handwritten as it made it more special, and that Mr B also had a heart. I slept with the heart the day it was received and had it with me when I did the eulogy. I am going to put the seeds on his grave”
- “I can’t describe the feeling when we got the box. Totally overwhelmed and speechless. Made us feel so connected and close to A – we were happy knowing he had a heart too”
- “As an employee of the Trust and someone with personal experience of dealing with the sadness of Covid, I would like to say, we are getting it right. My family found the bereavement box, containing a heart, some marigold flower seeds and a heart-warming message from the Trust comforting.”
Staff making the calls:
- “This service has really supported grieving families and friends who are feeling the sadness and loneliness of loss. So many people have thanked us for contacting them, providing help with any questions and passing messages of thanks to ward teams and providing a caring and compassionate approach at such difficult times. I feel that the development of this vital service underpins the core values of our organisation and the staff who work within.”
Staff supporting the administration:
- “During this scary and uncertain time it was very sad to see the daily large numbers of families who lost loved ones, however supporting this service felt like a very worthwhile small way we could help relatives and made us feel like we were playing our part.”
At the start of the pandemic impact was monitored via paper records unaware at that stage how long the project would run and how well received it would be. Once informed it would continue a more robust method of capturing the calls commenced to provide a more effective way of evaluating the service. Following discussion with Patient experience Quality Improvement colleagues we now have a section on the Datix reporting system, this will enable us to monitor outcomes, trends, and impact.
Standing Out
Our Trust believes this initiative is special as it places the relative’s wellbeing at the heart of the service. Being able to provide support for grieving families who may feel sadness and the loneliness of loss is a real honour and privilege. It is proactive service, provided for the NOK of all deceased patients – it embraces everyone – no one is left out. As far as we are aware no other Trusts provide this service, so ours is unique.
Main impact relates to the relatives’ experience with us as a Trust. The feedback has been incredibly positive. It has opened the 2-way dialogue with relatives which has been hugely appreciated. Trust colleagues have been open to hear concerns and deal with them in a timely manner to support families
Key elements that contributed to the success
- The staff who have been part of the team are from different areas and professions all coming together with a shared goal of supporting our bereaved relatives
- Being able to maximise the input from redeployed staff
- A very clear aim and structure where everyone knows what is expected of them
- The backing of the Trust from all levels.
Key Learning Points
The need to scope the specifics through a working group – considering:
- Workforce – nursing, General office, Clinical Governance administration, mortuary, support staff
- Funding – including any that can be accessed via charitable funds
- Storage – for the boxes
- Content of boxes and where the supplies will come from
- Hours of service – availability of staff
- Equipment – funding for laptops and telephones
- Day to day management – who will make calls, send boxes out, update deaths, maintain spreadsheet etc
- Governance – reporting/monitoring impact /GDPR / access to interpreters
Requires a business case detailing the service and where workforce will be sourced, potential costs and benefits. In addition, we recommend walking in the shoes of patients and their relatives – seek feedback regularly ensuring that it contains no bias and represents the extent of service users (e.g. use interpreters if needed).
Plan formal ways of evaluating the service and monitoring the impact from the start.
Case Study Resources
Watch the Presentation Here:
