Improving our Colorectal Cancer Pathway Patient Experience
Nottingham University Hospitals NHS Trust

Contact: James Blackwell - james.blackwell@nhs.net
Organisation
Nottingham University Hospital Trust – With 15,000 staff, we are one of the biggest employers in the city with a central role in supporting the health and wellbeing of our local population. We play a leading role in research, education and innovation. We have a national and international reputation for many of our specialist services, including cancer services and we are the tertiary referral centre for colorectal cancer in the region. We operate upon approximately 250 patients with colorectal cancer per year, with many more patients having contact with our department via diagnostic, treatment or surveillance pathways.
General Summary
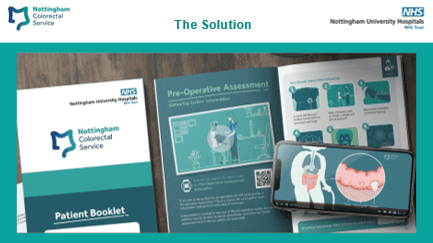
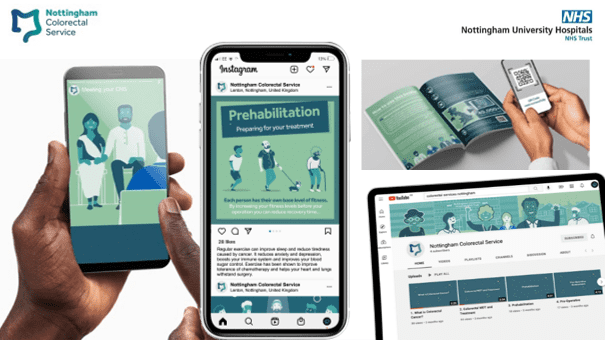
We have created bespoke, innovative and high-quality digital content (animations + social media) to guide and support patients through their colorectal cancer treatment journeys. Triggered by QR codes embedded in bespoke cancer patient pathway literature, this digital content condenses the huge quantity of patient literature previously given down to engaging, easy to share digital media.
Clear objectives and multi-level leadership have benefited this project. The governance group meets regularly and receives feedback from clinical champions within stakeholder working groups.
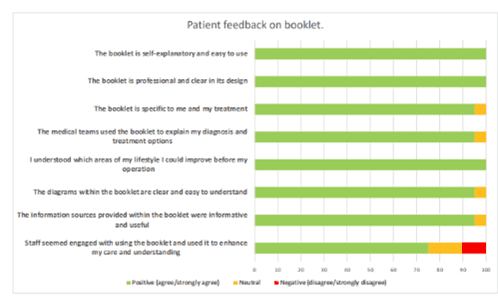
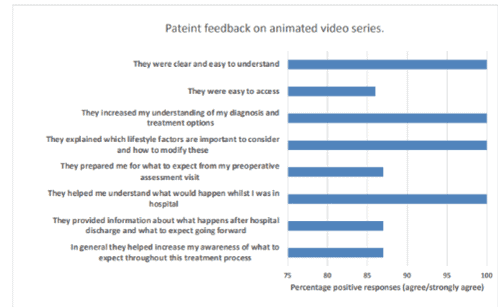
We report a 23% increased positive response rate (agree/strongly agree) to patient experience surveys. Our resources are in full clinical use and can all be updated in response to patient feedback and changes to clinical practice.
The design process centred around patient feedback and cancer survivor testimonials from the outset. We consulted multiple clinical stakeholders, working groups, addressed key elements of the pathway and connected discrete elements of the multi-disciplinary team. Since roll-out we have established continuous patient experience feedback.
Digital outputs from this project are fully transferable across the UK colorectal cancer population and indeed across other cancer groups. We have presented this project locally and are exploring dissemination via the colorectal expert clinical advisory group (ECAG) and Cancer Alliance.
Rationale
A pathway wide audit of our colorectal cancer service (externally commissioned via Johnson & Johnson) highlighted areas of excellence but also areas for improvement. The overall patient experience was highlighted as needing improvement. Concerningly, there were fundamental questions within the National Cancer Patient Experience survey where we fell below not only the national average but also standards we would want our patients or family to experience during contact with our service. For example Question 10: Patient completely understood the explanation of what was wrong, we scored 69% vs National average 79% and Question 12: Patient felt that treatment options were completely explained, we scored 78% vs National average 85%. We identified ten key questions requiring improvement having scored significantly below the national average. Our group felt that we should aspire to achieve 100% positive response rate to these questions.
We also saw opportunity to develop truly personalised stratified care, particularly during the period before treatment starts. In medicine this term is known as prehabilitation (like rehabilitation but before treatment). We wanted to develop an individualised risk assessment, targeting modifiable chronic health parameters, with measurable outcomes to target surgical risk factors.
We wanted to empower our patients to engage with their healthcare journeys. This requires clear communication, education about new diagnoses/how chronic disease increases their individual risk from surgery (and how we can support patients to modify this risk), whilst ensuring they feel fully informed and supported throughout. We wanted to improve the patients’ perception of continuity despite the huge number clinical/non-clinical staff involved in a patients’ care.
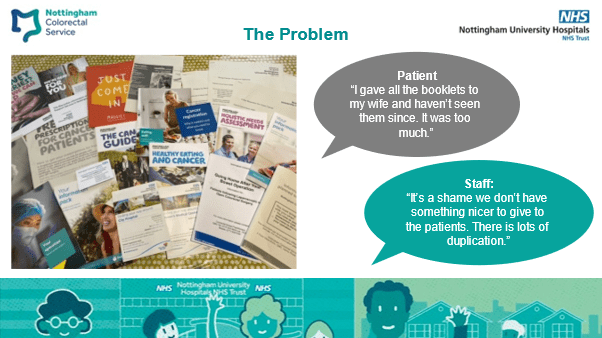
We are confident that our service delivers gold standard clinical care and it is important that this is reflected in the patient experience for both personal and professional pride across our workforce. Before this project patients received upward of >26 booklets upon receiving their cancer diagnosis. Many reported feeling overwhelmed by this and that the pages of written text were too much to digest.
We aimed to address the issues raised above by distilling current patient information into a single patient booklet, complimented by a series of informative/engaging animated videos. These resources guide the patient through their treatment journey from diagnosis to discharge and beyond. This addresses healthcare inequalities in those patients who have difficulties understanding written concepts and conveys large amounts of information in a visual format which is easily digested away from clinical environments.
Planning
A pathway wide audit of our colorectal cancer service (externally commissioned via Johnson & Johnson) highlighted areas of excellence but also areas for improvement. The overall patient experience was highlighted as needing improvement. Concerningly, there were fundamental questions within the National Cancer Patient Experience survey where we fell below not only the national average but also standards we would want our patients or family to experience during contact with our service. For example Question 10: Patient completely understood the explanation of what was wrong, we scored 69% vs National average 79% and Question 12: Patient felt that treatment options were completely explained, we scored 78% vs National average 85%. We identified ten key questions requiring improvement having scored significantly below the national average. Our group felt that we should aspire to achieve 100% positive response rate to these questions.
We also saw opportunity to develop truly personalised stratified care, particularly during the period before treatment starts. In medicine this term is known as prehabilitation (like rehabilitation but before treatment). We wanted to develop an individualised risk assessment, targeting modifiable chronic health parameters, with measurable outcomes to target surgical risk factors.
We wanted to empower our patients to engage with their healthcare journeys. This requires clear communication, education about new diagnoses/how chronic disease increases their individual risk from surgery (and how we can support patients to modify this risk), whilst ensuring they feel fully informed and supported throughout. We wanted to improve the patients’ perception of continuity despite the huge number clinical/non-clinical staff involved in a patients’ care.
We are confident that our service delivers gold standard clinical care and it is important that this is reflected in the patient experience for both personal and professional pride across our workforce. Before this project patients received upward of >26 booklets upon receiving their cancer diagnosis. Many reported feeling overwhelmed by this and that the pages of written text were too much to digest.
We aimed to address the issues raised above by distilling current patient information into a single patient booklet, complimented by a series of informative/engaging animated videos. These resources guide the patient through their treatment journey from diagnosis to discharge and beyond. This addresses healthcare inequalities in those patients who have difficulties understanding written concepts and conveys large amounts of information in a visual format which is easily digested away from clinical environments.
Public: We sough expert patient opinion from the colorectal expert clinical advisory groups (ECAG) patient liaison chair. This provided excellent insight into both his personal experience and lessons learnt on a regional level.
Delivery: We provided multiple staff education sessions frontline staff involved with the patient journey. We had a soft launch and three month pilot phase from February 2022. Cancer nurse specialists select appropriate patients to undergo the individualised risk assessment and they then receive the patient booklet.
Impact
An unexpected impact of this project has been upon staff groups not directly involved in clinical care (i.e. administrative support staff). They report greater understanding of the patient pathway and clinical terms used in patient correspondence. Staff report being proud to present patients with the booklet and believe it is a realistic representation of the care delivered.
Results (please see supporting evidence document):
Forty-three patients have received the booklet to date (22 patients having completed treatment and follow-up). We report a 23% increase in positive response rate (agree/strongly agree) to the ten key questions, which would have correlated to a mean of 17% higher than national average.
Patient quote: “After hearing ‘cancer’ I glazed over. The booklet and videos helped me understand what was happening to me and helped me cope with the whole experience.”
Patient quote after using booklet: “I did find it really useful that I could input into it as well as the clinical stuff. Doing the activity diary, saying I needed to be as fit as possible for the operation gave me the green light to get back running and boosting my fitness level up so I could be ready for the operation.”
Staff quote: “Patients have been able to show family members, ‘this is my diagnosis and this is my treatment plan going forward’. This have helped everyone’s understanding”.
Standing Out
This pathway wide intervention was designed to improve the continuity of care for patients and staff. Many projects impact discrete elements of the patient journey, we aimed for an over-arching intervention which connected many smaller elements, creating a seamless patient journey to enhance patients’ continuity of care.
Striving to deliver individualised stratified care with the patient at the centre. We believe that we have displayed intention and delivery of this key recommendation of the NHS Long Term Plan.
Thorough consultation process which included canvassing opinion, agreeing the common goal and designing interventions/solutions that worked for all. The sheer number of stakeholders makes this project stand out from others.
The overall professionalism and design quality of our resources has received high praise as this is not always experienced with the NHS. Clear objectives with the patient experience at the centre has allowed us to make impactful resources which are engaging and informative to patients. Bridging the gap between clinical knowledge and patient facing information is key to patients understanding their conditions and treatment options.
Key Learning Points
Patients told us what information they wanted – always involve patients from the outset, listen and give them what they want!
Patients retain a limited amount of information once they are given a cancer diagnosis. Information we provide often looks poor, is outdated or undigestible. We had to look critically at the information we were giving out to make positive improvements.
Ensuring patient understanding and expectations are set at point of diagnosis and then met throughout their treatment journey is key to maintain high patient experience levels.
Engage a large group of stakeholders – this allowed us to look at pathway wide issues, many of which were aspects of care traditionally separately delivered (i.e. preoperative assessment and post operative care).
Engaging all staff, with a common vision and goal, remembering that every patient contact counts maximised the patient experience impact of this project.
