King Cancer Collaborative Addressing Health Inequalities - Kings College Hospital NHS Foundation Trust
Winner – Cancer Experience of Care Award at PENNA23
Contact: Sola Banjo - sbanjo@nhs.net
Organisation
King’s College Hospital is a major teaching hospital and major trauma centre in Denmark Hill, Camberwell in the London Borough of Lambeth. King’s is a large local provider of diagnostic, surgical and other treatment services for common cancer. We diagnose over 4,000 new cancers a year across our main sites at Denmark Hill (King’s College Hospital), Orpington (Princess Royal University Hospital (PRUH)), and Beckenham Beacon.
King’s is a centre of excellence and regional service for:
- Haemato-oncology
- Liver cancer
- Neuro-oncology
King’s is a regional provider for breast and bowel cancer screening. We work with other leading hospitals, and in partnership with Guy’s and St. Thomas’s NHS Foundation Trust. We are part of South East Cancer Alliance (SELCA).
General Summary
The King’s / NHS England / Improvement collaborative work aimed to address Q7 of the national cancer patient experience survey (NCPES) addressing health inequalities and access to care. The King’s College Hospital project focused on our breast cancer population, where we have seen a significant variation between our adult patient population from a white background and patients from a Black and minority ethnic background, between 2015 and 2019.
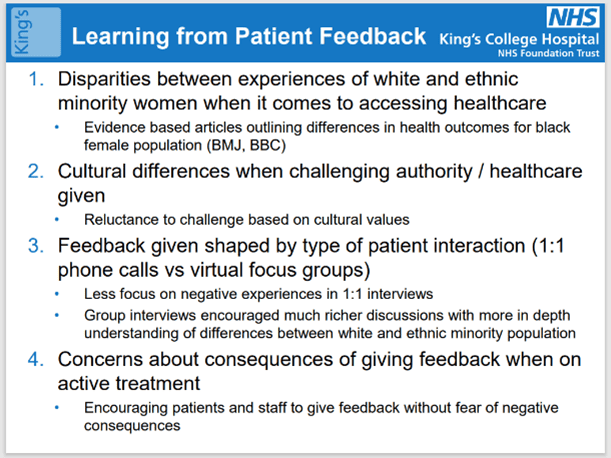
The project focused specifically on addressing patient’s understanding of diagnostic test results explained at the One Stop Breast Clinic. Following our patients feedback the team identified 5 changes/improvements which were successfully piloted and are being implemented.
The changes were co-designed with our patient representatives, clinical nurse specialists (CNS) senior leadership and wider SELCA colleagues.
Rationale
Results from the 2021 CPES showed a growing gap between our adult patient population from a white background and patients from a black and minority ethnic background. Therefore we looked to improve the experience of Black African patients at our Denmark Hill site and Asian patients at our Princess Royal University hospital site with suspected breast cancer at the time of referral. These groups represented the largest numbers of patients from ethnic minority backgrounds treated for breast cancer at both our main hospital sites. However our changes are expected to improve the experience for all patients accessing case at the King’s breast care unit.
Planning
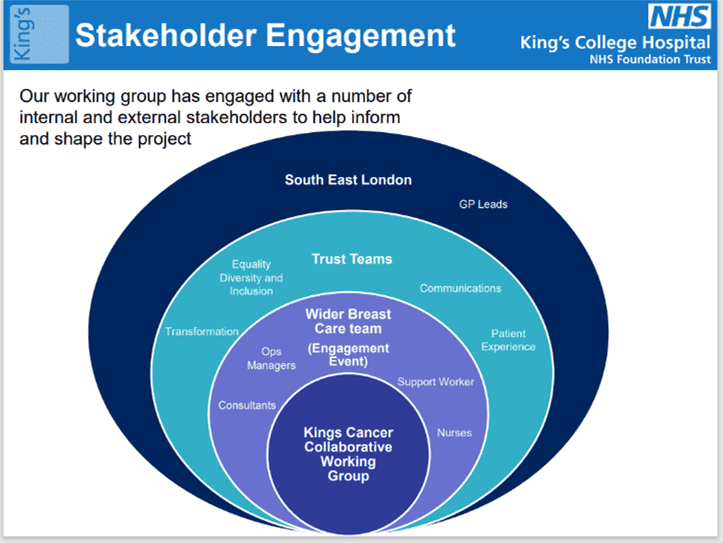
The project team comprised patients who had been treated at King’s for breast cancer, our cancer CNS leads, colleagues from radiology, communications, equality diversity and inclusion and patient and public involvement. In addition, improvement leads from our South East London Cancer Alliance (SELCA).
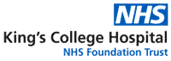
The Plan, Do, Study, Act (PDSA) model for improvement, was used to provide a delivery framework and co-production best practice has been the focus throughout the project. There were 4 PDSA cycles conducted to ensure the changes had the intended impact on patient experience. Thirty women participated in focus group discussions and surveys to establish our baseline.
89% of our breast cancer patients said the CNS and consultant explanation of their diagnostic tests was done with care and compassion. 11% said that we could make every interaction matter more. Therefore, we could not look at diagnostic test results in isolation but consider the wider experience of care at the point of access to cancer care. Therefore, the following change ideas have been co-designed with our lived experience partners:
- Changes to the language and content of urgent suspected cancer referral appointment letters
- Changes to messaging and language used on the Trust webpages to better reflect realities of attending the Breast Care Clinic at Kings
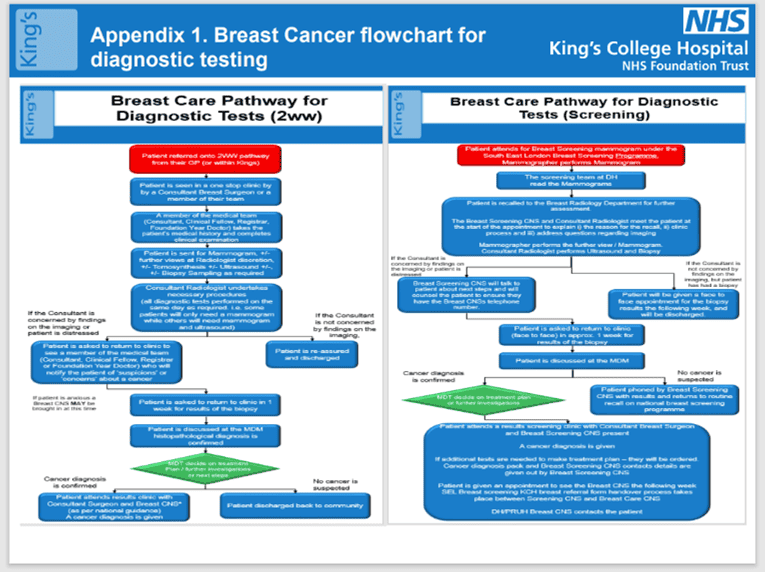
- Development of a flowchart explaining what patients can expect from the referral into the Breast Care Clinic until they receive their diagnostic test results
- Ensuring consistent presence of a clinical nurse specialist in the one stop clinic
- Development of a staff training video to increase awareness of cultural differences amongst our diverse populations and how patient’s experience affects their care
Success will be defined by having a target improvement of 10% in the 2023 NCPES scores.
Impact
The project team completed 44 patient follow-up interviews since implementing these resources. Feedback showed significant improvement in patients’ experience as well as highlighting further areas for improvement:
- Breast Care Flowcharts
- Consultation undertaken with local GPs to address how patients would access the flowcharts at the point of referral
- 10 patients who had a CNS present in their OSC upon receiving the results of their biopsy were surveyed about how useful they found it to have a nurse with them.
- All 10 patients said that they found the CNS presence helpful or very helpful when receiving their results14 patients given the flowchart
- 86% (12/14) of the patients said the flowchart was easy to understand and helped them to understand what tests to expect.2 patients said they did not understand the flowchart due to a learning disability and anxiety whilst waiting for her appointment.
Feedback highlighted the need for the development of easy read patient information which the project team have produced are starting to pilot
- Urgent referral letter
- 26 patients who were asked questions about their ease of understanding the content in the letter
- 87% (22 / 26) of patients who received a copy of the revised urgent suspected cancer referral appointment letter said they found the letter easy to understand
- . Updated breast care unit webpages
- Analysis of the webpages 2 months prior to the updated webpages going live (July 2022) and 2 months after (August – September 2022) shows a slight increase in page views from 979 to 1079
- The amount of time spent on the webpages has also increased from 3.05 mins to 3.17 mins.
- Staff training video addressing cultural differences awareness when communicating with patients from different backgrounds
- The video is available on the King’s learning and development platform. Staff are encouraged to complete as part of their induction. Within the first few weeks 22 staff members have completed this training
- The team were awarded the Great Idea Award by NHS England at the Cancer Experience of Care Improvement Collaborative Recognition Event, for easy spread and potential impact of this innovative idea
- CNS presence in one stop breast clinic (OSC)
- 10 patients who had a CNS present in their OSC upon receiving the results of their biopsy were surveyed about how useful they found it to have a nurse with them.
- All 10 patients said that they found the CNS presence helpful or very helpful when receiving their results
The Future
The project team have undertaken several measures to increase the likelihood of sustainability and are working with partners across SELCA and NHS England/Improvement, namely:
- The project team presented change ideas and our evaluation to the breast multi-disciplinary teams at our main hospital sites and at the SELCA breast tumour groups to ensure changes are understood and embedded in practice
- Rollout of multi-media communication to support patients around their diagnosis. For example, the team are working our digital transformation colleagues to pilot the sharing of urgent referral letter on a digital platform
- Continued use of the NCPES and the trust’s own Real Time Feedback Survey to monitor the impact of improvements and respond to changing needs
-
- Continuing quality improvement aimed at ensuring presence of CNSs in all breaking bad news (BBN) clinics
Promoting the staff training video on the King’s learning and development platform, encouraging staff to complete as part of staff induction. Within the first few weeks 22 staff members have completed this training. Also promoting amongst other health partners, including Macmillan, to share learning and opportunities for staff training
- The project team have been instrumental in influencing changes to the language and content of the urgent referral letters (beyond breast care) to better reflect patient’s views
- The team shared their learnings with SELCA and other breast teams, and more widely to other tumour groups multi-disciplinary teams including head and neck, lung and colorectal, more meetings being arranged. These colleagues have expressed interest in how they change practice to ensure the experience of patients from ethnic backgrounds can be improved at point of referral and throughout their pathway
- The project has also been presented at a national recognition event and launch event, hosted by NHS England / Improvement. Further presentations have also been made to the Pan London Lead Cancer Nurses groups
- The team have liaised with the learning disability charities and networks to co-design the easy read patient flowcharts
Standing Out
The key contributor to this project’s success is the co-design relationship between clinical staff and patients towards improvement. From the conception of the project, in reviewing NCPES data, designing patient questionnaires to gain a deeper understanding of where the issues might be, through co-designing all aspects of improvement, undertaking the PDSA cycle and reviewing data that has demonstrated success.
The project has also lead to the development of a staff training video, as outlined in section ‘impact and results achieved’. The video has received positive feedback from staff within the SELCA, NHSE/I and beyond, with 21 organisations making a request for the video to share with their staff.
Key Learning Points
Our key learnings include the below elements:
- Importance of ensuring executive level sponsorship prior to undertaking any large change project. This has been particularly valuable when tackling the need for changing behaviours and processes
- Good engagement needed from the whole project team, including representation across the whole multi-disciplinary team
- Importance of having lived experience partners/patient representatives involved at every step of the project from inception to close down
- Importance of understanding the problem, as evidenced by data collected both nationally and through locally conducted patient experience surveys, breaking this down to understand where variations exist between different groups of patients
- Importance of having flexibility to pivot on your original aim. Data may present a situation that is different to what you originally envisaged. As outlined in the above section ‘planning and delivery’.