Little Journey: A Children's Healthcare Procedure Preparation and Support Tool
Little Journey Limited

Contact: Dr Chris Evans - chris@littlejourney.health
Organisation
Little Journey is a health-tech SME founded in 2019. It was created based off the clinical and research experiences of Dr Chris Evans. Initially Little Journey was focused on supporting children through day case surgery but has now grown to supporting children undergoing multiple healthcare procedures and those participating in clinical trials. The team has grown from two people in 2020 to up to ten in early 2021 and is looking to increase to twenty staff at the end of the 2021. Little Journey licences its solutions to healthcare organisations, life science and contract research organisations, providing a tailored version to their needs. We are providing the NHS with a low-cost solution focusing on the international healthcare and contract research market for ongoing company sustainability.
General Summary
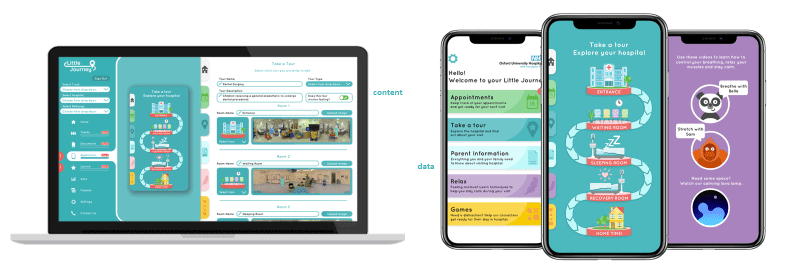
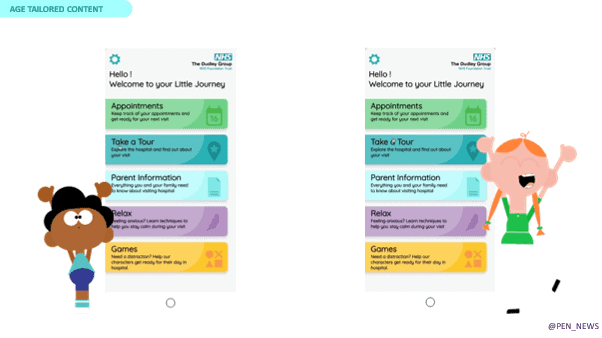
Little Journey is an end-to-end digital psychological preparation and support tool for children and their families undergoing a healthcare procedure. Consisting of a patient-facing mobile application (app) and hospital-facing web application (portal) that enables organisations to control the app in real time, Little Journey provides engaging, interactive and age-tailored content to families from the safety of their own home.
Little Journey was founded by Dr Chris Evans – a peri-operative anxiety management expert and NHS England clinical entrepreneur – with the aim of democratising health information. Working closely with key stakeholders, the platform has grown and evolved based on his research and understanding of key stakeholder needs.
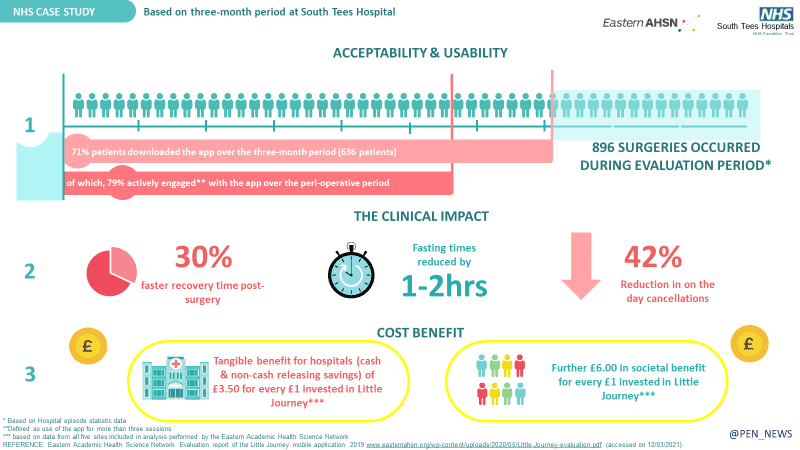
Little Journey has been configured to over 50 NHS organisations. A health economic analysis performed at five NHS organisations identified that 71% of patients verbally offered the app went on to use it, with 98% satisfaction. In addition, premedication rates, on-the-day cancellations, recovery times and fasting times were reduced providing cost-benefit to the hospital (£3.50 per pound invested) and society (£6.00 per pound invested).
Little Journey has since expanded to support families undergoing Endoscopy, phlebotomy and COVID swabs. It was accepted onto the NHS Innovation Accelerator program to increase adoption across the NHS.
Rationale
Little Journey is an end-to-end digital psychological preparation and support tool for children and their families undergoing a healthcare procedure. Consisting of a patient-facing mobile application (app) and hospital-facing web application (portal) that enables organisations to control the app in real time, Little Journey provides engaging, interactive and age-tailored content to families from the safety of their own home.
Little Journey was founded by Dr Chris Evans – a peri-operative anxiety management expert and NHS England clinical entrepreneur – with the aim of democratising health information. Working closely with key stakeholders, the platform has grown and evolved based on his research and understanding of key stakeholder needs.
Little Journey has been configured to over 50 NHS organisations. A health economic analysis performed at five NHS organisations identified that 71% of patients verbally offered the app went on to use it, with 98% satisfaction. In addition, premedication rates, on-the-day cancellations, recovery times and fasting times were reduced providing cost-benefit to the hospital (£3.50 per pound invested) and society (£6.00 per pound invested).
Little Journey has since expanded to support families undergoing Endoscopy, phlebotomy and COVID swabs. It was accepted onto the NHS Innovation Accelerator program to increase adoption across the NHS.
Planning
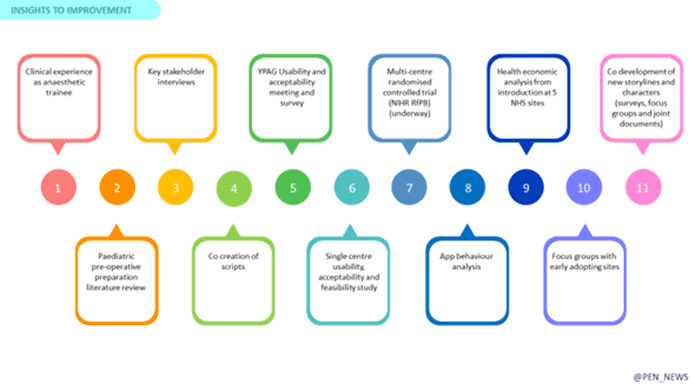
The first version of Little Journey was developed and launched in 2018 following an extensive double diamond co-development and design process through informal discussions, focus groups (both parent and Young Person advisory group (YPAGS)), as well as key stakeholder meetings. This version provided an age-tailored virtual reality tour of the rooms’ children would visit on the day of an operation. The storylines, characters and technology itself were assessed through two separate YPAGs.
Following its successful launch, we performed a single-centre usability and acceptability study which identified that parents act as gate keepers of healthcare information. It also identified that parents were using the app independently of their child to enable discussions about what would happen. This led to a second version of the application being co-developed which delivered drip-fed information articles to parents before and after the procedure. After the second versions launch, we held focus with early adopters identifying their desire to:
- create additional information pathways for common procedures such as MRI, Phlebotomy, etc
- collect and report patient reported outcomes for service improvement
- update information in real time
This has led to the significant expansion of our mobile- and web-facing applications to further benefit organisations and families. We have worked closely with organisations before and after launch to achieve ongoing customer success.
Impact
- Little Journey has been used over 35,000 times with over 350 app store reviews (4.7 rating). 97% of users rate the information provided as good or very good with an average use of 49 minutes and seven sessions.
- Our usability and acceptability study (IRAS number: 223644) surveyed parents of children undergoing ambulatory surgery to assess the usability and acceptability of the application and gain feedback, identifying that 100% of parents either agreed or strongly agreed it helped them talk to their child about the operation, that it helped prepare them for their child’s operation and that they would recommend to a friend before an operation. A follow-on multi-centre randomised controlled trial is currently underway in 10 NHS hospitals (IRAS number: 251219, REC:19/LO/0255).
- An independent health economic analysis assessing the cost-benefit of Little Journey’s introduction at five NHS Hospitals was performed. It identified a cost benefit to hospitals through lowering anxiety (reduction in premedication rates) and improving flow through the hospital (reduction in fasting times by one hour for liquids and two hours for solids, 30% reduction in the time spent in the recovery room and 42% reduction in on-the-day cancellations). Societal benefits were identified through an improvement in family’s quality of life and reduction in missed days of work.
- Belfast children’s hospital reported a 30% reduction in parent perceived anxiety levels in children with Autism and ADHD undergoing daycase dental surgery.
Standing Out
Several patient-facing applications have been created with the aim of preparing children to come to hospital. Typically, they attempt to support children of a single age group over a wide range of procedures using generic, inflexible content with insufficient depth. Little Journey changes this.
Through provision of a solution designed for both children and their parents, Little Journey promotes discussion and learning across the child’s social network, while provision of content over the whole peri-procedure period makes the information digestible and understandable. For children, the delivery of multi-faceted immersive, engaging and age-tailored content from virtual reality tours, therapeutic games and relaxation exercises promotes ongoing engagement and makes the preparation enjoyable.
A core component of Little Journey is the flexible, modular, hospital portal that puts hospitals directly in control. By enabling organisations to configure the mobile application to their local patient pathways, we create a personalised solution to increase engagement. The ability to update content in real time prevents incorrect and out of date information dissemination.
A key element contributing to the success of Little Journey has been its co-design with key stakeholders including children, families and healthcare professionals. Similarly, creating continual learning loops through formal research and real-world evidence has ensured the solution stays relevant and evidence driven. Finally, the pandemic has heightened the need for a digital solution that can be continually updated to support families from the comfort and safety of their own home.
Key Learning Points
- There is no one-size fits all solution and human behaviour requires variation to engage and satisfy everyone. This is particularly relevant when it comes to health behaviours and information preferences to better understand how people will respond to health information.
- Keep co-design at the core and listen
- Combine subject matter experts, healthcare professionals, children and families voices together to create the ideal solution but also identify how this solution should be implemented.
- Focus is often placed solely on the efficacy of the intervention rather than its ability – or the desire – for it to be implemented into routine care, resulting in a research-to-practice gap. Close this gap through implementation science focusing not only on the effectiveness of an intervention but the cost-effectiveness, security, implementation strategy and interoperability.
- Balance the need for accuracy and speed by generating data from both standard clinical trial methodologies and real-world evidence.
- Actively seek the unheard voice to address health inequalities. Young person advisory groups naturally self-select their participants with those with chronic illness, interests in healthcare or healthcare professional relatives. The voice of the person who needs the intervention most is often never heard.
- Continue to seek feedback and learn. Create continual learning loops to iterate and improve the solution. It is never finished.