Little Voices - Walsall Healthcare NHS Trust
Winner – Communicating Effectively with Patients and Families And Overall PENNA 2023 Winner

Contact: garry.perry1@nhs.net
Organisation
Walsall Healthcare NHS Trust is an integrated Trust and provider of NHS acute care, serving a population of 286,700, providing inpatient and outpatient services at the Manor Hospital as well as a wide range of services in the community. Walsall Manor houses the full range of district general hospital services under one roof. The £170 million development was completed in 2010 and the continued upgrading of existing areas ensures the Trust now has a state-of-the-art Critical Care Unit, Neonatal Unit, Obstetric Theatre, and Integrated Assessment Unit facilities. Work has also been completed on our new multi-million pound new Urgent and Emergency Care Centre which houses a new Emergency Department (including Children’s Emergency Department), co-located Paediatric Assessment Unit, Acute Medical Unit and Urgent Care Centre. This opened officially in June.
General Summary
As our youngest patients, children have a unique perspective on their wellbeing. Their views and experiences can differ from what we, as adults, assume or expect. When we listen carefully to children, their experiences and opinions can enrich and even alter the course of our decisions and the plans that we make. Little Voices helped inform and support our ambition towards delivering care in a setting that is child-friendly and equitable for all children. The amplification of the children’s voice, children of such a young age provided meaningful participation that was not just child led but provided for an understanding of what accessing care is really like for a child seen through their eyes and not that of a parent or carer. Our initiative opened an opportunity to shape both place and purpose which has resulted in actions that demonstrated we have listened and acted on the feedback our ‘little voices’ have given. The importance of hand hygiene, mealtimes that matter, play that is engaging, reducing fear and anxiety are set to improve the way that we involve children in the care that is provided to them and ‘all about me’ becomes the norm in practice.
Rationale
Following the 2021 Children and Young Peoples (CYP) survey, the CYP Division launched an improvement programme called back to basics. There were several drivers for this including post-pandemic recovery (some aspects of service provision such as play had been restricted), a worsening position in several responses to questions than the previous survey and an identified need to re-focus on patient and family involvement about the way services would change and develop in future.
Led by the CYP Senior Leaders and the Patient Experience team, the use of patient feedback was seen as crucial to how we could learn and improve from the lived experiences of those who use access our services. As a start existing mechanisms of providing feedback were strengthened including the implementation of bedside posters using QR codes and the introduction of a digital mystery patient scheme.
The children’s ward identified a Clinical Support Worker Patient Experience champion to work with families identifying areas for improvement based on the feedback received including promotion of the ‘Tops and Pants’ line. One thing that was missing was the voice of the child and involvement with children was seen as something that is often overlooked in favour of more conventional methods such as surveys and the feedback given primarily by parents/guardians. This is where Little Voices was borne to include the child’s voice in re-designing and improving services for children and young people whilst also validating article 12 of the United Nations Convention on the Rights of the Child – the right to an opinion, for it to be listened to and taken seriously.
Planning
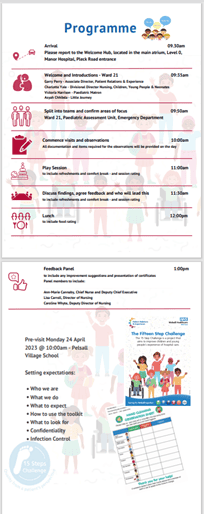
The Patient Experience team firstly secured a partnership with a local primary school – Pelsall Village, who identified a group of children aged 7-10 to work with us. Planning sessions were held at the school and the children worked independently with the headteacher identifying what mattered most to them when accessing healthcare. The children reviewed the 15 steps toolkit and re-designed the approach and in turn produced a new child friendly booklet for use when carrying out a visit. The children looked at what information they would want to see when attending the hospital or if they were admitted. Their feedback and insight shaped the installation of a new ward welcome board. In addition, ‘all about me’ boards were designed with a view to personalising and including the child and parent/guardian in their plan of care.
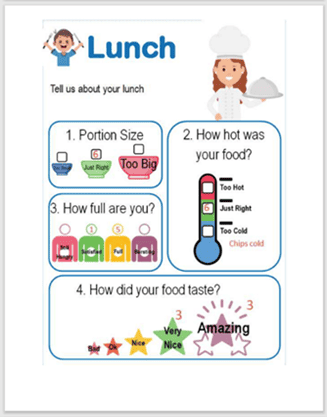
In preparing for the 15 steps inspection visit, we held a ‘what to expect’ workshop attended and led by the Patient Experience Team, Play Specialist and Head of Infection, Prevention and Control. The workshop explored the children’s feelings associated with being poorly and sought to understand more about patient anxiety and worry when attending the hospital. The children learned about infection control and how quickly germs can spread and the importance of washing hands. In addition, they learned about staff roles and who they would likely encounter in a hospital setting. The children also co-designed a simple hand hygiene checklist for use by patients in hospital aimed at reducing the risk of cross infection and hospital acquired infections. The children also participated in a hand hygiene test where bacterium was grew following the passing around to each other of a soft toy. The Play specialist spent time listening to the children explain their likes and interests so that a hospital play session could be designed around individual and collective needs ahead of the 15 steps visit.
Impact
Back to Basics’ was the improvement plan that was a catalyst for this innovative piece of work. This meant a focus on responding to the less favourable outcomes of the 2021 CYP National survey and to attest that we were improving the recommendation scores in the Friend and Family Test and associated themes.
Using a themed analysis of paediatric FFT comments, the trust can track changes in positive and negative comments over time. Since January 2023, inpatient paediatric services have received consistent positive comments about staff attitude, with PAU seeing an increase in comments throughout the period to June. On average, paediatric services have maintained 40% or more positive comments received during the period specifically mentioning staff attitude in a positive light. This improvement in staff attitude, whilst following an improving trend across inpatient areas, is proportionately higher than the trust inpatient average of 30%.
From a review of complaints and concerns there has been a 70% reduction from 21/22 to 22/23 (30 and 9 respectively) and of the mystery patient comments received all were positive in relation to staff courtesy, environment and facilities, dignity and respect and involvement in care (themes from the national survey).
In addition, a clinical group was set up to put into effect the actions arising from the Little Voices + feedback. The motivation is to utilise this group to track and monitor improvement actions and to mirror survey the questions against those in the National Survey as we prepare for this year’s sampling. This renewed focus on patient and carer involvement also led to paediatric services being open to include volunteers in their engagement with children and their parent/guardians and we now have four young volunteers working across the service – called EWE’s (Enhancing the Ward Experience) who work on placement with us in partnership with Walsall College as part of their protected services course.
The Future
The Little Voices team will be returning in December on a ‘you told us we have’ visit and to also assess the children’s outpatient area. We have a plan for annual involvement in different workstreams and to date these include the re-design of the children’s outdoor play area and involvement in recruitment processes using a concept called the ‘Children’s desert island interview process’. We have since held a youth forum with a focus on mental health and to support the development of a Walsall wide strategy for young people’s wellbeing. The intention is to form additional school partnerships and plan for the development of a mealtime, playtime, and sleep time charter for the in-patient areas. We are currently working with the Little Journey App team to develop our own pre-hospital package of information. This will help reduce anxieties for pre-hospital and pre-theatre, it will orientate families to the ward before they arrive, and it can be used to share information to support care at home. The Little Voices team have already reviewed the app and given it their ‘nod’.
Standing Out
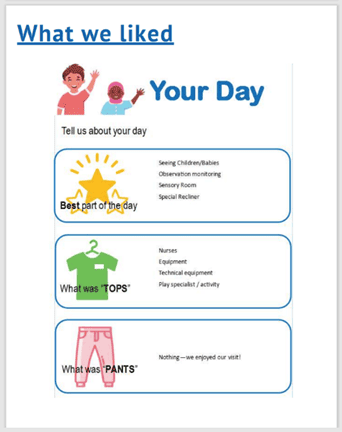
This is a unique approach that has ignited excitement on a multi-professional level in the importance of levelling up the involvement of children in service design and improvement. It’s different because it has been child led, its different because it affirms the core principle of article 12, its different because it provides staff with insight that enhances practice and adds greater depth of understanding from a child’s perspective. This is a different approach because it’s not conventional in terms of the way we would usually obtain feedback and act on it, furthermore organisations tend to focus patient involvement on those considered more able to speak for themselves or of adolescence. The key elements of our success have been the partnership with a school, this is because sometimes children are not in the hospital setting long enough for meaningful engagement to take place or are too poorly, however they have all either had or have familial experiences of coming into or accessing hospital services. Another success marker has been the creativity of the programme to adapt to the children’s viewpoint when it has differed to that which we anticipated. This has led us to act on areas which we did not consider to be a problem at the time – sometimes this is a simple solution such as changing a mirror in the sensory room which was viewed by a child to have potential danger. The collaborative team approach between the CYP team, Patient Experience, Infection and Prevention and Emergency Department was another success measure.
Key Learning Points
Of importance is the investment of time in building the relationship and interest of the children. Expect the unexpected as once the children are engaged, they can often take an interest in the things that you may not have thought of such as a relaxation chair, themed side room and child friendly linen. Make it interesting too – let them take an observation, sit in the back of an ambulance, and use a stethoscope – it’s all about the stethoscope. From a staff perspective it’s all about team collaboration and a multi-disciplinary approach, in the planning of 15 steps take time to risk assess what the children could inadvertently be exposed to which is why the pre-planning visits are also crucial, and smile – the children respond positively to kindness and are reciprocal when the visit is made fun.