Outpatient Assessment Clinics @ Dorset Health Village - Dorset's 'Think Big' Initiative
University Hospitals Dorset

Contact: Jonathan Wright - jonathan.wright@uhd.nhs.uk
Organisation
Dorset ICS is a collaborative partnership between the Health and Social Care providers across Dorset. It covers a population of circa 800,000 people, with a high proportion of people being over the age of 65. There are also 11 areas in Dorset which have been identified as being some of the most deprived areas nationally.
Dorset Integrated Care System: (Comprising Bournemouth, Christchurch and Poole Council, Dorset Council, Public Health Dorset, Dorset County Hospital NHS Foundation Trust, Dorset HealthCare University NHS Foundation Trust, South Western Ambulance Service NHS Foundation Trust, Primary care estate (79 practices, involving 18 primary care networks), University Hospitals Dorset NHS Foundation Trust).
General Summary
Winner – Integration and Continuity of Care & Partnership Working to Improve the Experience
To develop pioneering, high volume community outpatients assessment centres (OACs) seeing tens of thousands of people across Dorset. Specifically incorporating the lessons learned from the rapid deployment of mass vaccination clinics and Nightingale hospitals throughout the Covid-19 pandemic, providing centres quickly, effectively, safely and within locations where it has the most impact for Dorset’s population. Working in partnership across the system our centres offered a range of vital services to help tackle health inequalities exacerbated by the Covid-19 pandemic creating a new and innovative model of hospital treatment for patients by developing a culture of prevention within the OACs. This focused on delivering three key outputs:
- Improving access to diagnostics and screening services, reducing waiting times and significant backlogs to reduce clinical risk, enable earlier identification to improve prognosis and available options for condition / disease management
- Increased opportunity for MDT approach to clinic delivery and integration of services from different NHS organisations / partners. (e.g. community and acute co-location)
- Focus on waiting well for care, prehabilitation, and support with long term conditions via access to VCSE organisations, health coaches, social prescribing
All delivered ensuring patients and clinicians remained the driving force behind the design and implementation.
Rationale
As a result of the Covid-19 pandemic hospitals were running at 100% capacity and were forced to reduce elective activity, significantly increasing waiting lists. There was also a high proportion of the population postponing treatments or not seeking advice to reduce their risk of being exposed to Covid-19, potentially causing future health problems. Local data shows that when comparing elective to non-elective admissions in Dorset, there is a clear difference in healthcare utilisation, with people from more deprived backgrounds accessing less elective and more emergency care. It was identified that without intervention there would be further detrimental impact on our citizens health
Dorset’s solution was to establish the Health Village, a series of Outpatient Assessment Centres (OAC) located within densely populated areas, with the greatest level of need for outpatient and screening services. By moving some services closer to the community we had the opportunity to not only reduce waiting times and increase access, but also enable earlier identification of disease and improve outcomes for our patients.
The impact of Covid has demonstrated the importance of good health and wellbeing and that disparities do exist between different communities. Therefore, the centres provide opportunities to design new clinical pathways and new ways of operating outpatient and screening services to ensure wellbeing services are fully integrated and embedded to provide advice, information, and support for people to make healthy behaviour changes to improve the health of our residents.
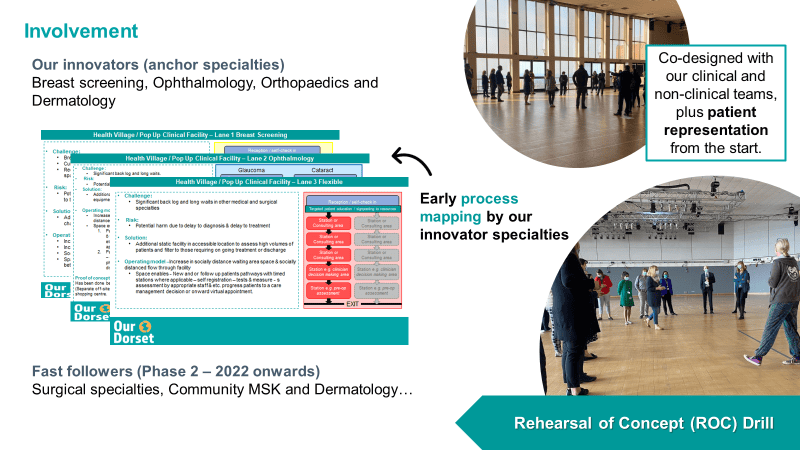
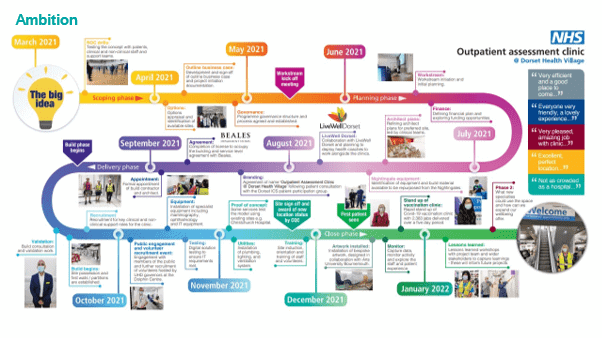
Planning
The planning and delivery of the project brought together patients, staff and wider stakeholders from various teams within Dorset ICS and beyond. To enable the phenomenal pace of delivery of facilities, strategically placed in the heart of communities, the team used militarily planning techniques including the Rehearsal of Concept (ROC) Drill. By bringing together patient and staff from across all areas of the ICS (e.g., digital, operational, clinical, admin) the group was able to ‘walk the patient journey’ and map the requirements for both the facility and patient flow, adopting a test, adapt and evolve philosophy throughout .
Our clinicians took leading roles in working with colleagues from multiple workstreams, including with architects to design the physical space and flow of patients moving around the clinic.
Patients, carers, and the public played a crucial role in the planning process and regular touchpoints were embedded in the project delivery from the start. Besides regular engagement with ICS patient engagement group, patient governors (representing the voice of the local community) played an active role in project delivery as leaders within the communications and engagement workstream, relaying feedback from their wider patient networks.
Public engagement events also took place – a 3-day event held in Poole enabled the project team to engage with the public around plans for the Health Village, enabling views and concerns to be captured, 3D models for the facility to be shared and wider communication to take place.
Members of the public in volunteer roles have been actively engaged from the outset and continue to play a crucial role in supporting the patients who attend the facilities.
Impact
Our benefits workshop, held with stakeholders across the project, identified benefits across several domains. Metrics within these domains continue to be evaluated to measure impact.
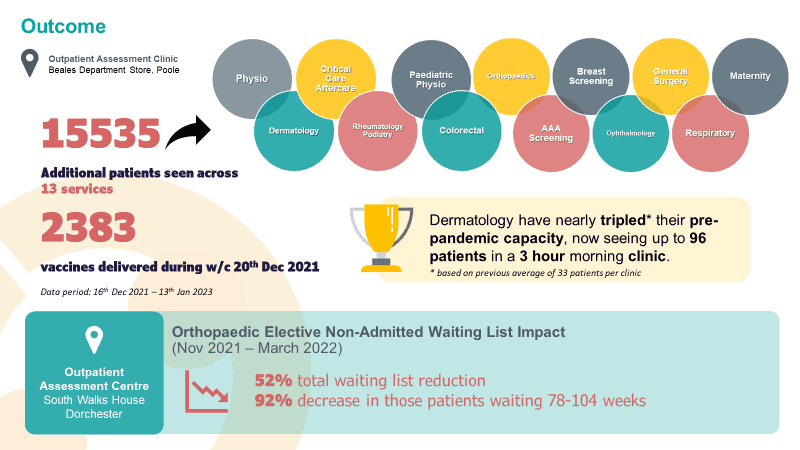
Some of the key successes so far:
Since opening, we have seen over 10,000 patients. The Orthopaedics speciality has seen a 92% reduction in 78–104-week waiters and a 31% uplift in activity, including 25% increase in appointment utilisation. With over 280 Livewell interventions to help patients ‘wait well’ for their definitive treatment. In addition, over 2,000 COVID-19 vaccinations were administered at the site in the week prior to Christmas 2021 in rapid response to the government mandate.
Analysis of patient feedback at the OACs indicates that 96% of patients had a positive experience. The increased satisfaction has improved outpatient attendances and increased confidence, whilst also ensuring that our workforce time, resources, and expertise is utilised in the most efficient and productive way.
The way in which we were able to design, build, implement and operate these facilities at pace and during the height of the Covid-19 pandemic has created and accelerated a test bed for new and different ways of working; informing the way in which services can be delivered at acute hospital sites and across the healthcare system for better efficiency.
Integration of several services under one roof, reducing touchpoints for our patients by ensuring the wellbeing services were given the physical space to incorporate into the patient journey. Since opening, the Health villages, continue to onboard and incorporate additional service provisions, with Poole now offering eight speciality services as well as ongoing wellbeing provision.
The Future – We have already secured a further twenty-year lease for our assessment centre at Dorchester along with additional funding for the next 3 years to incorporate a ringfenced 24 bed orthopaedic ward as well as ongoing wellbeing service provision.
Bringing care closer to peoples’ homes and working with patients to design the provision of services ensures that services are fully embedded, sustainable for our current and future populations and put patients at the heart of design to improve access and equity of care.
We have adopted a quality improvement approach to the way in which we deliver our Health villages ensuring we maintain a proactive approach to seeking, listening and responding to public and patient feedback. This includes our “You said, We did” engagement approach (see supporting evidence), which has already made significant changes to our patient experience.
Dorset ICS is committed to the delivery of the Health Village and as we continue to deliver benefits to outpatients on the high street, we will help build the case for further sustainability. Services are being supported by strengthened networks of GP practices, offering patients a wider range of services. As well as aligning commissioning intentions across the ICS partners for sustainability. We are actively seeking further funding to continue the initiative for further years and in future locations across Dorset through the Community Diagnostic Centre programme.
Standing Out
The unprecedented situation brought about from the Covid-19 pandemic brought a unique opportunity to ‘think differently’ about how we delivered our services. The Health Village has left a legacy for innovation in Dorset, notably some of the key areas that made this area stand out:
– The use of military planning techniques – Dorset was able to rapidly bring together and engage stakeholders across a number of partner groups and build a team culture that enabled rapid delivery of the project
– The redeployment of Nightingale equipment – supported the sustainability and financial aspects of the project. Architect plans were based on availability of equipment and material, led by clinical teams.
– Patient leadership – the embedding of patient engagement throughout course of project and leadership roles within project governance structure enabled ongoing ‘sense-checking’ against plans for facility and link to patient voice.
– Co-location of health and wellbeing services within acute services – for the first time, Dorset physically co-located health coaches and social prescribing alongside acute services which enables a more holistic approach to delivering patient care.
– Partnership with retail – repurposing existing estate enabled rapid delivery of facilities and the creation of unique NHS – retail relationships to support both population outcomes and socioeconomic development of local community.
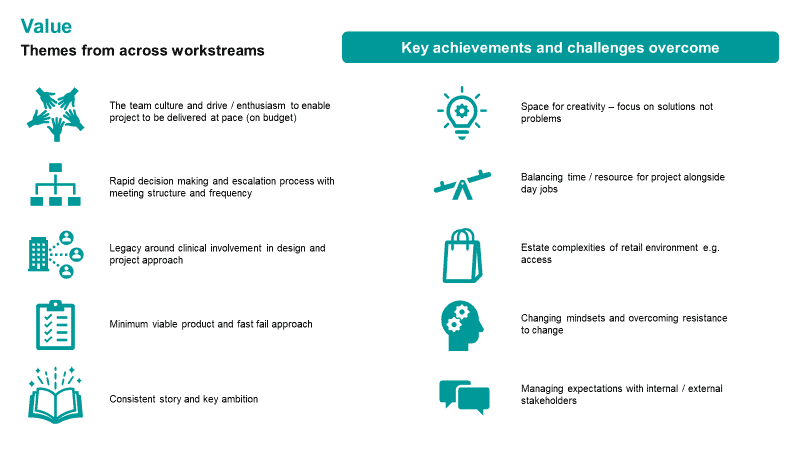
Key Learning Points
A full lessons learned evaluation has taken place, engaging stakeholders across the project and including representation from our patients to enable key themes to be identified.
From this evaluation the following lessons have emerged:
– Clearly defined programme governance and roles and responsibilities– this enabled rapid decision making and escalation plus early identification of risks and issues to enable rapid delivery.
– Providing space for creativity and allowing evolution of ideas – ensure all stakeholder groups are heard, focus on solutions not problems and embed the voice of patients and clinicians throughout the project.
– Develop a Minimal Viable Product (MVP) model – whereby decisions are made on the principle of whether it will meet the required outcomes, this enables focus on end goal, remaining within tight deadlines and budget, and helps reduce scope creep.
– Regular touchpoints and face-to-face planning – enabled rapid formation of team and culture, alignment of shared vision across partners, maintained momentum and helped overcome resistance to change.
– Agility in running different due processes in parallel – by thinking innovatively around how due processes associated with cross sector partnership working can be facilitated in a more rapid and agile manner to enable ambitious timescales to be achieved.
– Learnings – applying expertise and methodologies from across different industries and internal partners to inform transformation and delivery of new services.
